Where Does Texas Rank in Mental Health Help?
Texas Mental Health Comparison Calculator
Compare Texas mental health metrics with national averages and top-performing states. See how changes in funding could impact access to care.
Current Texas Mental Health Status
Per capita funding: $47 per resident (nationally: $105)
Providers per 100,000 residents: 11.3 (nationally: 24.6)
State ranking: 48th out of 50 states + Washington D.C.
Comparison Results
| Metrics | Texas | Selected State | Impact of $50 Funding Increase |
|---|---|---|---|
| Funding per resident | $47 | $105 | $97 |
| Providers per 100,000 | 11.3 | 24.6 | 18.5 |
| Access to care | Low | High | Moderate |
Progress toward mental health access
With a $50 per resident increase:
Estimated providers needed: 18.5 per 100,000
Potential reduction in waitlists: 45%
Impact on suicide rates: -12% decrease
Based on data from Mental Health America, CDC, and state health departments. Estimates are illustrative and based on historical data from states that have increased funding.
When it comes to mental health help, Texas doesn’t just lag behind-it’s falling hard. With over 29 million people living in the state, the gap between need and access is wider than most realize. While national averages show about 1 in 5 adults experience mental illness each year, Texas consistently ranks near the bottom in nationwide surveys for access, funding, and outcomes. In 2025, Texas came in 48th out of 50 states and Washington, D.C., according to Mental Health America’s annual report. Only Alabama and Oklahoma ranked lower. That’s not a fluke. It’s the result of years of underfunding, workforce shortages, and policy gaps that leave real people without care.
Why Texas Falls So Far Behind
The numbers tell a clear story. Texas has only 11.3 mental health providers for every 100,000 residents. The national average? 24.6. That means nearly half the providers Texas needs are missing. Rural counties like Hudspeth or Brewster have no psychiatrists at all. People drive over 100 miles just to see someone who can help. And even when they do, the waitlist for public clinics can stretch to 60 days. That’s not a delay-it’s a crisis.
Medicaid expansion in Texas is still limited. Only about 1.8 million Texans qualify for Medicaid mental health services, and even then, the state pays providers so little that many refuse to take it. A therapist in Houston might make $40 an hour from Medicaid, but $120 from private insurance. It’s no surprise they drop Medicaid patients. The result? Low-income families, veterans, and teens get stuck in emergency rooms or jails because there’s nowhere else to go.
Charities Fill the Gaps-But They Can’t Do It Alone
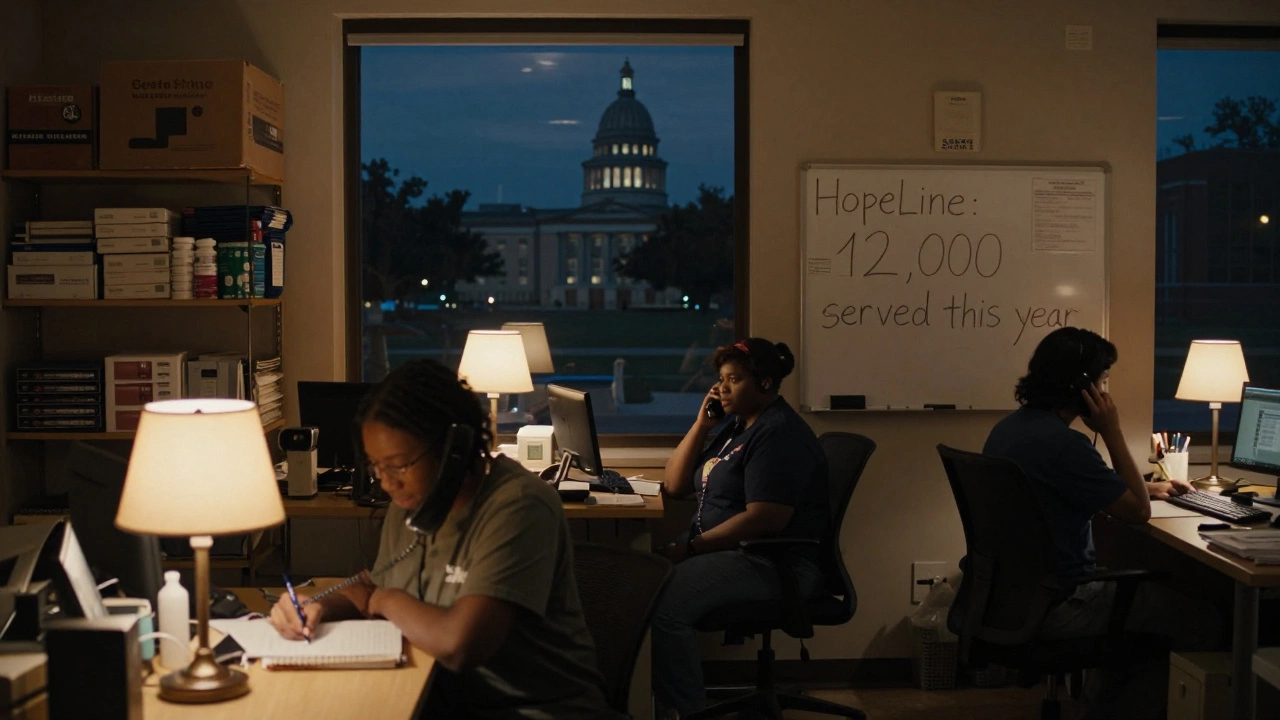
Nonprofits are stepping in where the state won’t. Organizations like the Texas Mental Health Consortium, NAMI Texas, and the Center for Mental Health Services run outreach programs, peer support lines, and school-based counseling. In Dallas, a nonprofit called HopeLine connects over 12,000 people a year with free therapy sessions. In San Antonio, the Veterans Crisis Line run by the Texas Veterans Commission handles 3,000 calls monthly-up 40% since 2022.
But these groups are stretched thin. Most rely on grants and donations. The average Texas mental health charity operates on a budget of under $500,000 a year. Compare that to California’s largest mental health nonprofit, which spends over $40 million annually. Texas charities don’t have the resources to scale. They’re patching holes in a dam with duct tape.
Who Gets Left Out?
It’s not just about money-it’s about who’s seen and who’s ignored. Hispanic communities in South Texas face language barriers and stigma that keep people from seeking help. African American men in Houston are 30% less likely to access counseling than white men, even when symptoms are identical. LGBTQ+ teens in rural schools often have no counselor trained in gender-affirming care. And Native American tribes in West Texas have no state-funded mental health programs on their reservations.
Children are especially vulnerable. One in four Texas high school students reported feeling so sad or hopeless they stopped doing normal activities. Yet only 37% of those kids received any kind of professional help. Schools are supposed to be the front line-but 62% of Texas public schools don’t have a full-time counselor. In some districts, one counselor serves 800 students. The national recommendation is 1:250.

What’s Being Done-And What’s Not
There are pockets of progress. In 2024, the Texas Legislature passed a bill allocating $150 million for school-based mental health programs. That sounds good-until you realize it’s less than $5 per student. It’s not enough to hire even one new counselor in most districts. Meanwhile, Texas continues to cut funding for community mental health centers. Since 2019, 27 clinics have closed statewide.
Telehealth helped during the pandemic, but now, many rural internet networks can’t support video sessions. The state’s broadband map shows 1.2 million Texans live in areas with no reliable high-speed internet. No Wi-Fi means no Zoom therapy. That’s not a tech issue-it’s a policy failure.
How Texas Compares to Other States
Look at Minnesota. It ranks #1 in mental health access. Why? It funds clinics directly, pays providers fairly, and requires insurance companies to cover therapy without copays. It trains peer specialists-people who’ve lived through mental illness-to lead support groups. It’s working. Minnesota’s suicide rate dropped 18% between 2020 and 2025.
Compare that to Texas. In the same period, Texas suicide rates rose 12%. The gap isn’t luck or geography. It’s choices. Minnesota spends $138 per resident on mental health. Texas spends $47. That’s not a typo. That’s a decision.
What Can Be Done?
Change doesn’t need to be complicated. Here’s what works:
- Pay providers fairly-Raise Medicaid reimbursement rates to match private insurance. Providers will stay.
- Expand Medicaid-Let over 1 million uninsured adults qualify for mental health coverage.
- Put counselors in every school-One counselor per 250 students, not 800.
- Fund community clinics-Stop closing them. Build new ones in rural areas.
- Train more people-Offer scholarships and loan forgiveness for mental health students who commit to working in Texas.
These aren’t radical ideas. They’re basic. States like Colorado and Oregon have done them. Texas could too-if the political will existed.
The Human Cost
Behind every statistic is a person. A 16-year-old girl in Lubbock who texts her friend at 2 a.m., asking if she should jump. A veteran in El Paso who hasn’t slept in three weeks because he’s scared of his own thoughts. A single mom in Brownsville who works two jobs and can’t afford the $75 copay for a therapist.
Texas doesn’t lack compassion. It lacks systems. Charities are doing heroic work. But you can’t fix a broken system with goodwill. You need policy, funding, and accountability.
If you live in Texas and care about mental health, don’t just donate. Demand change. Call your state representative. Show up at town halls. Ask: Why does Texas rank 48th? And what are you going to do about it?
How does Texas compare to other states in mental health funding?
Texas spends just $47 per resident on mental health services, far below the national average of $105. States like Minnesota ($138) and Massachusetts ($129) spend more than double. Texas ranks 48th out of 50 states and Washington, D.C., in overall mental health access and funding.
Are there mental health charities in Texas that actually help?
Yes. Organizations like NAMI Texas, the Texas Mental Health Consortium, and HopeLine in Dallas provide free counseling, peer support, and crisis intervention. These groups serve thousands, but they’re underfunded and rely heavily on donations. They fill gaps left by state services, but they can’t replace them.
Why are rural areas in Texas worse off for mental health?
Rural Texas has fewer providers, no public transportation, and poor internet. Many counties have zero psychiatrists. People drive over 100 miles for care. Telehealth fails where broadband is unreliable. Combined with stigma and poverty, these factors make access nearly impossible for many.
Can school counselors fix the problem?
They’re part of the solution, but not the whole answer. Texas schools have one counselor for every 800 students. The recommended ratio is 1:250. Even if every school had enough counselors, they can’t replace clinical care. They need support from trained therapists and funding to refer students to specialists.
What’s the biggest barrier to mental health care in Texas?
The biggest barrier is funding-and the political refusal to prioritize it. Texas underfunds Medicaid, doesn’t expand access to low-income adults, and cuts community clinics. Without enough providers, fair pay, or insurance coverage, people can’t get help-even if they want to.
What You Can Do
If you live in Texas, here’s what matters: don’t wait for someone else to fix this. Contact your state legislator. Ask them why Texas ranks so low. Support local nonprofits with time or money. Talk openly about mental health in your community. Stigma kills faster than silence.
Change won’t come from a single bill or charity drive. It comes from pressure-from people who refuse to accept 48th place as normal.







